
Автор: Кэролайн Браун, Джорджио Иотти
Дата: 08.07.2022
При применении искусственной вентиляции легких часто наблюдается асинхронность между пациентом и аппаратом ИВЛ (1, 2).

Асинхронность вдоха и выдоха пациента и аппарата ИВЛ может принимать различные формы (это может быть, например, раннее или позднее переключение с вдоха на выдох, аутотриггирование, двойной триггер или слабые усилия) и, как было показано, влияет на результаты лечения (
Концепция анализа кривых давления в дыхательных путях и потока для выявления дыхательных усилий и определения их времени была впервые описана почти тридцать лет назад (
Ключевым элементом данного исследования было применение систематического метода на основании общих физиологических принципов и ряда конкретных, определенных заранее правил («метода анализа кривых») для анализа кривых давления в дыхательных путях и потока. Все пациенты находились на ИВЛ в режиме поддержки давлением; каждому был установлен пищеводный катетер. Метод применялся для анализа кривых давления в дыхательных путях и потока, полученных с помощью проксимального датчика; в качестве эталона использовались показатели давления в пищеводе (Pes). Для каждого пациента три участника исследовательской группы общей численностью четыре человека (в нее входили три старших врача и один ординатор) анализировали только кривые потока и давления, в то время как другой исследователь анализировал как кривые потока и давления, так и кривую пищеводного давления. Дыхательные движения были классифицированы следующим образом: дыхательные движения при «нормальной» поддержке аппарата, при аутотриггировании, при двойной триггере и при слабых усилиях. В случае «нормальной» поддержки также оценивались случаи незначительной асинхронности (задержка триггирования, раннее переключение с вдоха на выдох, позднее переключение с вдоха на выдох).
Первичной конечной точкой была доля спонтанных усилий, определенная методом анализа кривых. Ко вторичным конечным точкам относились согласованность результатов определения существенной и незначительной асинхронности, полученных методом анализа кривых и эталонным методом исследования, а также показатель согласия экспертов по поводу метода анализа кривых.
Всего было зафиксировано 4426 вдохов. На основании эталонных измерений пищеводного давления 77,8% из них были идентифицированы как вдохи, правильно обнаруженные аппаратом ИВЛ, 22,1% – как слабые усилия и 0,1% – как вдохи в результате аутотриггирования. Методом анализа кривых удалось обнаружить 99,5% спонтанных усилий и все, кроме одного, вдохи в результате аутотриггирования. Также отмечалась высокая степень согласованности результатов, полученных эталонным методом и методом анализа кривых при определении разных дыхательных движений: осуществленных при поддержке аппарата, в результате аутотриггирования, двойного триггера и слабых. Показатель асинхронности был рассчитан как сумма слабых, осуществленных в результате аутотриггирования и двойного триггера дыхательных движений, разделенная на общее количество вдохов, и составил 5,9%, причем методом анализа кривых и методом измерения пищеводного давления были получены одинаковые показатели. Общая продолжительность асинхронности, рассчитанная как время, в течение которого аппарат ИВЛ и пациент не были синхронизированы, разделенное на общую продолжительность мониторинга, составила 22,4%, при этом на долю незначительной асинхронности пришлось 92,1% общей продолжительности. Показатель согласия экспертов по поводу классификации дыхательных движений также был очень высоким.
В более чем 90% случаев методом анализа кривых удалось с достаточной точностью определить начало и конец дыхательных усилий, что также позволило правильно идентифицировать тип «незначительной» асинхронности – в результате задержки триггирования, раннего и позднего переключения с вдоха на выдох.
В настоящем исследовании представлены некоторые важные выводы. Согласно исследователям, метод анализа кривых позволяет клиницистам обнаруживать чрезвычайно высокий процент спонтанных усилий и точно оценивать время активности пациента. Даже при незначительной асинхронности данный метод является надежным и воспроизводимым. Важность результатов подчеркивается еще одним выводом, сделанным по итогам исследования: большая часть продолжительности асинхронности при вентиляции с поддержкой давлением (PSV) была связана с незначительной асинхронностью.
Результаты исследования не только демонстрируют воспроизводимость метода анализа кривых (высокий показатель согласованности экспертов), но также указывают, что обучение этому анализу в соответствии с предварительно определенным систематическим методом играет ключевую роль. Имеющиеся данные свидетельствуют, что клинический опыт лечения пациентов на ИВЛ не обязательно предполагает способность распознавать асинхронии, которая в целом у врачей реанимационного отделения довольно низкая (
Авторы приходят к выводу, что проксимальные кривые давления в дыхательных путях и потока воздуха содержат достаточную информацию для точной оценки активности пациента и взаимодействия пациента и аппарата ИВЛ, если применяется соответствующий систематический метод анализа, например «метод анализа кривых».
Технология IntelliSync®+, которой оснащены аппараты ИВЛ Hamilton Medical (
Полный список цитируемых материалов см. ниже: (

В справочной карте приведен обзор наиболее распространенных типов асинхронностей, а также описаны их причины и способы выявления.
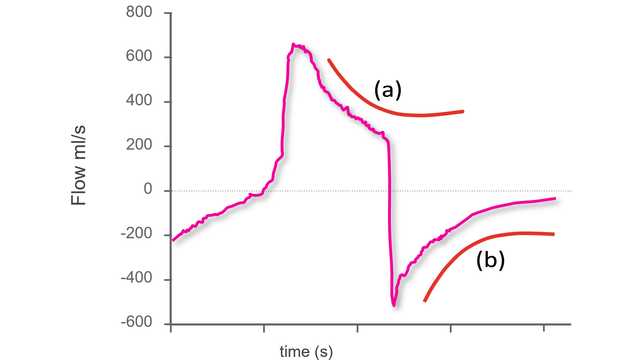
Первое действие для выявления асинхронностей с помощью стандартных кривых аппарата ИВЛ – понимание, что собой представляет синхронное дыхание во время вентиляции с поддержкой давлением.
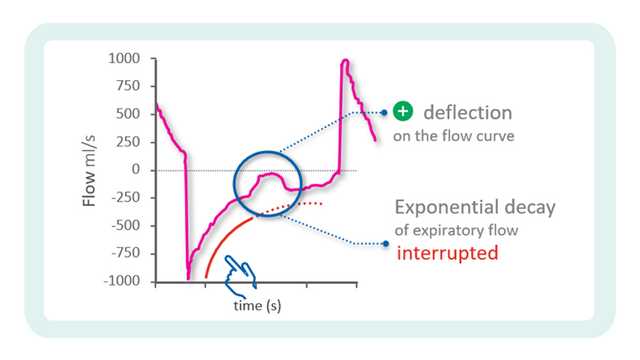
В предыдущем блоке практических советов мы начали рассматривать определение асинхронностей с помощью кривых на аппарате ИВЛ.